|
|
|
|

This article was originally published on Kaplan Test Prep’s Calling All Nurses
Who needs chocolates, flowers, and sentimental cards when your life is one big extraordinary love affair? In honor of Valentine’s Day, we’ve asked fellow-RN Damion to express his affection for nursing in a love letter:
Dear Nursing,
You have captured my heart. I think about you every morning when I first wake up, and I think about you every night before I go to sleep. You are ever present in my dreams, and you are always in my prayers.
You can be intimidating, but to those who love you, you are inspiring. You are complex, ever-changing, and require a great deal of passion and discipline to master, but you are worth the effort. You are a career that demands relentless self-sacrifice, but you provide some of the greatest rewards known to mankind.
You have provided me with many valuable lessons and offer me something new to learn every single day. You hold me accountable and inspire me to reach my full potential, constantly challenging me to grow and develop myself both personally and professionally in my career.
Most days, we are in perfect harmony, but some days we don’t quite see eye to eye. You make me laugh and cry—often both at the same time. Occasionally, I find myself needing a break from you, in desperate need of some “me time.” But when I feel your absence for too long, I miss you terribly. I am reminded that passion for any career involves a level of suffering, so I welcome it gladly.
We have had some amazing adventures together over these past seven years, and I am looking forwards to a lifetime of memories. This journey with you has been one of the most extraordinary love affairs in my life, and I wouldn’t trade it for any other career.
Happy Valentine’s Day to you—my heart, my passion, my legacy!
-Damion
New Website and Blog Host coming soon at http://www.thenursespeak.com... stay tuned for great things to come!!!
 Since the launching of Nurse Speak Blog in June of last year, I have had the pleasure of working with, and being supported by many wonderful people and organizations both in and out of the Nursing Profession.
Since the launching of Nurse Speak Blog in June of last year, I have had the pleasure of working with, and being supported by many wonderful people and organizations both in and out of the Nursing Profession.
The Nurse Speak Blog has received an overwhelmingly positive response from an international audience, ranging from eager nursing students, to that of healthcare policy makers.
So I just wanted to take a moment to give a big THANKS to all of those who have shared, posted, reblogged, and added the Nurse Speak Blog site to their blogroll lists!
Thank you very much, and I look forward to continuing to make a positive impact within the nursing profession!
Firstly, a HUGE thank you to my dear friend Crystal, creator and author of sincerelycrys.com – a fabulous lifestyle blog, for her help in getting started. Although her assistance was brief, her insight was extremely valuable!
Thank you to many members of the
View original post 273 more words
 Along with the challenges RNs face come immeasurably more benefits. In our attempt to celebrate and highlight what drives a registered nurse to compassionately care for their clients—we share monthly inspirational quotes from RNs with our colleagues and those who advocate for the recognition those in nursing deserve.
Along with the challenges RNs face come immeasurably more benefits. In our attempt to celebrate and highlight what drives a registered nurse to compassionately care for their clients—we share monthly inspirational quotes from RNs with our colleagues and those who advocate for the recognition those in nursing deserve.
This this January edition, we asked three nurses to provide words of wisdom for new graduate RNs. Here are their words of inspiration:
“Your first year of nursing will prove to be challenging. At times, you may experience mixed emotions and will be conflicted between what you believe what should be happening in the delivery of client care versus the reality of the situation. Just remember one thing—you are in control of how you respond to each situation, and your duty is to protect and serve your clients at all costs.” —Nurse Educator of 8 years
“Get ready to be flexible like never before. You may experience many situations that cause some anxiety or stress, and you have to be prepared to handle these situations professionally and efficiently. At times, doctors may yell at you, CNAs will not always be there to help, and patients will not always be grateful for your selfless care. You have to be able to quickly work through these negative situations and not take everything personally. At the end of the day, you have to do whatever is best for your patients.” —Cardiac RN of 27 years
“Never be afraid to ask questions! I cannot emphasize this enough, especially since I have seen so many new graduate nurses struggle because they weren’t asking questions. I have been an RN for over 30 years and I ask questions every single day. If there is ever one single hesitation, you should stop what you are doing and ask for guidance, or clarification, especially from doctors and specialists. Remember, when in doubt, check it out!” —RN of 34 years
Best Wishes!
-Damion
This article was originally published on Calling All Nurses
One of the greatest challenges we face in healthcare today is the ability to balance
healthcare quality with low costs. With current changes in healthcare reimbursement, there is a focused effort on moving to value-based purchasing, also known as pay for performance.
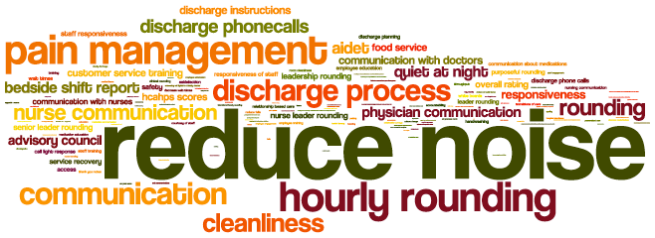
In part one of this two-part article, we defined Hospital Value-Based Purchasing, along with the HCAHPS Survey. In part two, we will identify the nursing implications for practice regarding Hospital Value-Based Purchasing and provide tips for nurses to positively impact their clients’ perceptions on the care received during an inpatient stay.
According to RN.com (2017), in hospitals, nurses are the primary caregivers 24 hours a day, seven days a week for patients; therefore, the impact on client satisfaction overall is directly related to the nursing care delivered. An entire section of the HCAHPS survey is dedicated to questions directly related to the clients’ perception of nursing care received while in the hospital. Many of the nursing HCAHPS items relate to effective communication and interaction. The nurse is in a perfect position to facilitate communication, not only with clients and nursing staff, but with other disciplines as well.
Some HCAHPS items relate to communication about medications and discharge teaching, as well as ask about the client’s understanding of the information provided. The nurse has the opportunity to provide information about medications and discharge expectations throughout the hospitalization. To validate the effectiveness of teaching, the nurse uses the teach back method, by asking the client to state their understanding of the information provided.
HCAHPS also measures the client’s perception of pain management—specifically how long they had to wait in pain before a nurse provided pain relief interventions. Finally, some of the HCAHPS items relate to cleanliness and quietness of the patient care environment, and nurses can enhance their communication with other team members that can impact the client care environment, such as reducing noise levels at the nurse’s station.
Many hospital-acquired conditions are directly influenced by nursing care. An example could include the progression of pressure ulcers that may develop with insufficient turning and repositioning and poor nutrition. Hospitals are no longer reimbursed for treating Hospital Acquired Conditions, and therefore it is extremely important that if the condition is present upon admission that fact is well-documented as well as any incidents that occur during the hospitalization.
Here are some strategies to positively impact patient’s perceptions and prevent Hospital Acquired Conditions:
Best Wishes!
-Damion
This article was originally published on Calling All Nurses
 One of the greatest challenges we face in healthcare today is the ability to balance
One of the greatest challenges we face in healthcare today is the ability to balance
healthcare quality with low costs. With current changes in healthcare reimbursement, there is a focused effort on moving to value based purchasing, also known as pay for performance.
In this two part article, we will define Hospital Value-Based Purchasing, the HCAHPS Survey, the Nurse’s Role in Hospital Value-Based Purchasing, and provide Tips for Nurses to positively impact their patient’s perceptions on the care received during an inpatient stay.
Defining Hospital Value-Based Purchasing
According to the Centers for Medicare & Medicaid (2017), Hospital Value-Based Purchasing (VBP) is part of the Centers for Medicare & Medicaid Services’ (CMS’) long-standing effort to link Medicare’s payment system to a value-based system to improve healthcare quality, including the quality of care provided in the inpatient hospital setting.
The program attaches value-based purchasing to the payment system that accounts for the largest share of Medicare spending, affecting payment for inpatient stays in over 3,500 hospitals across the country.
Participating hospitals are paid for inpatient acute care services based on the quality of care, not just quantity of the services they provide. Congress authorized Inpatient Hospital VBP in Section 3001(a) of the Affordable Care Act.
Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) Survey
Objective and subjective data collected from patients after discharge from the hospital is then evaluated using the Hospital Consumer Assessment of Healthcare Providers and Systems survey. According to HCAHPS (2017), the intent of the HCAHPS initiative is to provide a standardized survey instrument and data collection methodology for measuring patients’ perspectives on hospital care.
There are three goals of the HCAHPS survey. First, the survey is designed to produce comparable data on the patient’s perspective on care that allows objective and meaningful comparisons between hospitals on domains that are important to consumers. Second, public reporting of the survey results is designed to create incentives for hospitals to improve their quality of care. Third, public reporting will serve to enhance public accountability in health care by increasing the transparency of the quality of hospital care provided in return for the public investment.
With these goals in mind, the HCAHPS project has taken substantial steps to assure that the survey is credible, useful, and practical. This methodology and the information it generates are available to the public.
After the data has been collected and evaluated, nurse managers use the data to collaborate with hospital administrators in order to create programs that empower nurses to improve the patient experience. The goals then become that their unit’s individual patient satisfaction scores should meet or exceed the national standard.
Stay tuned for Part 2 where we will discuss the Nurse’s Role in VBP, and will provide Tips for Nurses to positively impact the perceptions of their patients during an inpatient hospital stay.
Best Wishes!
-Damion
This article was originally published on Calling All Nurses
 In our ever-changing health care system, nurses are consistently challenged to maintain strong ethics in nursing in the face of a fast-paced work environment. In this series so far, we defined the nine Provisions of Nursing Ethics, and we highlighted three of the most common ethical dilemmas nurses face.
In our ever-changing health care system, nurses are consistently challenged to maintain strong ethics in nursing in the face of a fast-paced work environment. In this series so far, we defined the nine Provisions of Nursing Ethics, and we highlighted three of the most common ethical dilemmas nurses face.
In the final part of this three part series, we are providing easy strategies for you to incorporate these nine Provisions of Nursing Ethics into your nursing practice:
Provision 1: The nurse practices with compassion and respect for the inherent dignity, worth, and unique attributes of every person.
Strategy: Treat your clients like you would want to be treated, or as if they are a loved one. This will help you give compassionate care at all times.
Provision 2: The nurse’s primary commitment is to the client, whether an individual, family, group, community, or population.
Strategy: Remember that your State Issued RN license is a contract between you and your clients. When it comes to the delivery of safe client care, your supervisor and/or facility administration takes the back seat until you have safely completed all required care.
Provision 3: The nurse promotes, advocates for, and protects the rights, health, and safety of the client.
Strategy: Using the nursing process greatly assists the nurse in upholding this provision. Knowing what is best for the client comes from interviewing, assessing client data, and observations made. Always think of the anticipated outcomes for the client, and you will naturally promote, advocate for, and protect the client.
Provision 4: the nurse has authority, accountability, and responsibility for the nursing practice; makes decisions, and takes actions consistent with the obligation to promote health and provide optimal care.
Strategy: This is similar to Provision 2, where the RN is required to dedicate themselves to the client while in their care, and assume all responsibility of care provided. The best way to practice within Provision 4 is to always do your best, and when mistakes occur, own them and seek guidance right away.
The nurse owes the same duties to self as to others, including the responsibility to promote health and safety, preserve wholeness of character and integrity, maintain competence, and continue personal and professional growth.
Strategy: Taking care of oneself is easier said than done, however it is essential to the delivery of safe and effective client care. Here is a great Nursing the Nurse series that provides tips for maintaining optimal health as a nurse.
Provision 8: The nurse, through individual and collective effort, establishes, maintains, and improves the ethical environment of the work setting and conditions of employment that are conducive to safe, quality health care.
Strategy: The best way to help create an ethical work environment is to set an example by role modeling ethical behavior, and holding others accountable. Be sure to know your facility’s procedure for reporting unethical behaviors in the event that a report needs to be made.
Provision 7: The nurse, in all roles and settings, advances the profession through research and scholarly inquiry, professional standards development, and the generation of both nursing and health policy.
Strategy: Besides returning to school for an advanced degree in nursing, becoming a member of a professional nursing organization or a nursing journal is an easy way to advance your profession through scholarly inquiry. Also, as you move throughout your nursing career, finding yourself in leadership, education or health policy positions will ensure that you are building professional standards and shaping the policies that guide nursing practice.
Provision 8: The nurse collaborates with other health professionals and the public to protect human rights, promote health diplomacy, and reduce health disparities.
Strategy: Community Nurses are the primary resource for upholding Provision 8, however even if you are not working in the Community Nursing specialty, you can volunteer and get involved on a larger scale.
Provision 9: The profession of nursing, collectively through its professional organizations, must articulate nursing values, maintain the integrity of the profession, and integrate principles of social justice into nursing and health policy.
Strategy: The best way to meet the ethical requirements of this provision is by upholding nursing values and demonstrating integrity in your daily practice.
Best Wishes!
-Damion
This article was originally published on Calling All Nurses
 Along with the challenges RNs face come immeasurably more benefits. In our attempt to celebrate and highlight what drives a registered nurse to compassionately care for their clients—we share monthly inspirational quotes from RNs with our colleagues and those who advocate for the recognition those in nursing deserve.
Along with the challenges RNs face come immeasurably more benefits. In our attempt to celebrate and highlight what drives a registered nurse to compassionately care for their clients—we share monthly inspirational quotes from RNs with our colleagues and those who advocate for the recognition those in nursing deserve.
As the new year approaches, we look back and reflect on what we’d like to improve upon over the next 365 days.In this New Year’s edition, we asked three RNs to share their New Year’s Resolutions:
“I really struggled with workplace conflicts over this past year. As a result, I have decided that my New Year’s resolution will be to organize and lead a staff retention and support committee for our unit. With a team of people working on enhancing the workplace environment through an organized committee, I am sure we will easily identify areas of concern, and work together to provide a solution. 2017 will be a better year for sure!” —Intermediate Care RN of 4 years
“After reflecting on this past year of nursing, I have found myself experiencing compassion fatigue more than ever before. I even took a brief leave of absence to get myself in a better place emotionally so that I could give my all to my clients when I returned. I love being a nurse, and I never want to feel like I just don’t care ever again. Therefore, I’ve decided that my New Year’s resolution will be to teach classes on compassion fatigue and provide strategies on how nurses like me can work through it. I truly believe that if nurses are prepared to handle compassion fatigue, they will do a much better job at being available both physically and emotionally for their clients.” —Telemetry RN of 7 years
“2016 has been a really great year for me in nursing. As a new graduate RN since Spring of this year, I have learned so much and have really been able to get comfortable in my abilities to independently care for clients. What I would like to improve upon is my delegation strategies. I find it so hard to delegate tasks to the nursing support staff, especially when they’ve been working in patient care a lot longer than I have. So for my New Year’s Resolution, I will work on improving my delegation skills by resourcing the senior nursing staff, and by reading publications on effective delegation strategies.” —Medical Surgical RN of 6 months
Best Wishes!
-Damion
This article was originally published on Calling All Nurses
 In our ever-changing health care system, nurses are consistently challenged to maintain strong ethics in nursing in the face of a fast-paced work environment.
In our ever-changing health care system, nurses are consistently challenged to maintain strong ethics in nursing in the face of a fast-paced work environment.
In part one of this series, we introduced the nine provisions within the code for ethics in nursing as defined by the ANA. In part two of this series, we will identify three of the most common ethical dilemmas nurses face in today’s challenging practice:
Client freedom vs nurse control
Nurses are well-educated in their skill set and aware of the best clinical course of action when it comes to helping their clients meet anticipated outcomes of treatment. But when a patient refuses to accept the plan of care, or denies treatment recommended by the healthcare team, nurses are faced with an ethical dilemma—allowing the client autonomy to make decisions and refuse treatment, regardless of the fact that the nurse understands that refusal of treatment may result in client harm.
The battle of beliefs
Evidence-based and empirical knowledge to a nurse might be completely subjective to a patient with a particular set of religious or personal beliefs. Certain religions and belief systems forbid procedures which could mean the difference between life and death. For example, in some cultures and religions, blood transfusions—even life-saving ones—are unacceptable. If the nurse attempts to explain the benefits of the procedure versus the risks of opting out of treatment, their actions can be received by the client and/or family as disrespectful and offensive. Similar to patient freedom versus nurse control, regardless of the nurse’s beliefs or values, the nurse faces the ethical dilemma of withholding life-saving treatment on the basis of another’s religion or belief system.
Resource management
Nurses are often helping clients when they are at their worst, and in many cases, it is with a patient that is in a medically futile state. As healthcare costs continue to rise, nurses are charged with the task of containing costs of services provided. As a result, nurses are challenged with maintaining a big picture perspective while also delicately handling intensely personal situations on a day-to-day basis. In situations like these, the nurse faces the ethical dilemma of helping families make financial decisions regarding the continuation or discontinuation of treatment, while understanding that a grieving family may lose hope during this very emotional and intense decision-making process.
Stay tuned for part three of this series where we will offer easy strategies for incorporating the nine provisions of ethical nursing standards into your daily practice.
Best Wishes!
-Damion
This article was originally published on Calling All Nurses
 In our ever changing health care system, nurses are consistently challenged to maintain safe and ethical nursing practice standards in the face of a fast paced work environment. One of the best ways to ensure that we are practicing within these ethical guidelines is to start by understanding what they mean.
In our ever changing health care system, nurses are consistently challenged to maintain safe and ethical nursing practice standards in the face of a fast paced work environment. One of the best ways to ensure that we are practicing within these ethical guidelines is to start by understanding what they mean.
According to the American Nurses Association (ANA), the Code of Ethics for Nurses was developed as a guide for carrying out nursing responsibilities in a manner consistent with quality in nursing care and the ethical obligations of the profession. There are 9 provisions in the code of ethics for nurses that encompass the standards in which nurses are to practice.
In part one of this three part series, we will introduce you to the 9 provisions within the code for ethics for nurses. Here are the 9 provisions as defined by the ANA:
Provision 1 -The nurse practices with compassion and respect for the inherent dignity, worth, and unique attributes of every person.
Provision 2 -The nurse’s primary commitment is to the patient, whether an individual, family, group, community or population.
Provision 3 -The nurse promotes, advocates for, and protects the rights, health, and safety of the patient.
Provision 4 -The nurse has authority, accountability, and responsibility for nursing practice; makes decisions; and takes actions consistent with the obligation to promote health and provide optimal care.
Provision 5 -The nurse owes the same duties to self as to others, including the responsibility to promote health and safety, preserve wholeness of character and integrity, maintain competence, and continue personal and professional growth.
Provision 6 -The nurse, through individual and collective effort, establishes, maintains, and improves the ethical environment of the work setting and conditions of employment that are conducive to safe, quality health care.
Provision 7 – The nurse, in all roles and settings, advances the profession through research and scholarly inquiry, professional standards development, and the generation of both nursing and health policy.
Provision 8 -The nurse collaborates with other health professionals and the public to protect human rights, promote health diplomacy, and reduce health disparities.
Provision 9 -The profession of nursing, collectively through its professional organizations, must articulate nursing values, maintain the integrity of the profession, and integrate principles of social justice into nursing and health policy.
Stay tuned for part two of this series where we will identify some common ethical dilemmas that nurses face, and in part three, we will offer easy strategies for incorporating these provisions of ethical nursing standards into your daily practice!
Best Wishes!
-Damion
This article was originally published on Calling All Nurses